Diabetic Retinopathy: A Key Role for Ocular Oximetry?
Diabetic retinopathy (DR), the most common complication of diabetes, is a retinal disease, characterized by ischemia, neovascularization and edema.

Clinically, there are two types of DR: non-proliferative and proliferative. Non-proliferative diabetic retinopathy (NPDR) represents an earlier stage of the disease and is marked by increased vascular permeability and capillary occlusion. Patients may be asymptomatic; however, on exam, microaneurysms, hemorrhages and exudates in the retina may be observed. Proliferative diabetic retinopathy (PDR) is a more advanced stage of the disease; its hallmark is neovascularization, the formation of new and abnormal blood vessels in response to poor perfusion. PDR can lead to vitreous hemorrhage or tractional retinal detachment, potentially leading to severe vision impairment. (1)
Diabetes is projected to affect 640 million adults around the world by 2040. DR affects 1 in 3 diabetics and is the leading cause of vision loss in adults of working age. (2) By 10 years after diabetes diagnosis, 71-90% of Type 1 and 67% of Type 2 patients will show signs of DR. (3)
Strategies to Prevent Blindness by DR
There are three broad approaches in preventing blindness as a result of DR. The first is primary prevention, whereby lifestyle modification, pharmaceuticals, and systematic screening are employed in an effort to prevent DR. Secondary prevention attempts to diminish DR progression through systemic risk factor control, regular eye screenings, and the implementation of evidence-based guidelines. Finally, tertiary prevention in preventing blindness from DR involves the use of ophthalmic treatments such as laser photocoagulation and surgery to manage active disease. In order to address blindness from DR globally, we must focus mainly on measures that address primary and secondary prevention.(2)
Importance of Early Diagnosis
It has been estimated that DR starts to develop up to 7 years before a diabetes diagnosis. Therefore, DR may often be identified at the first visit following diabetes diagnosis.(4) Once DR is diagnosed, it is imperative to mitigate disease progression to minimize the risk of blindness. For example, according to the Early Treatment of Diabetic Retinopathy Study (ETDRS) and the Diabetic Retinopathy Study (DRS), the administration of timely laser photocoagulation has the potential to reduce severe visual loss by 90%. Still, timely identification and treatment of DR remain a challenge for health care providers. (3)
A major breakthrough in DR management would be the ability to measure oxygen saturation levels in order to assess metabolic changes before damages occur.
Diagnosis of Diabetic Retinopathy
Let’s look into how we detect and monitor the disease today.
Ophthalmoscopy
When a patient with diabetes is seen by an eye care professional, dilated ophthalmoscopy is done. This test, performed by an ophthalmologist or optometrist, has a sensitivity of 65.7% and a specificity of 93.8% for detecting signs of DR. (3)
Fundus Photography
Photographing the retina can help to identify and document the presence or absence of DR in a particular patient. The static nature of photography enables more certainty in observation. The wider field of view of a photograph relative to the image in direct ophthalmoscopy affords the examiner a broader overview of the eye. Serial image comparison is also possible, allowing for the visualization of change over time.
Optical Coherence Tomography
Optical Coherence Tomography (OCT) is another tool used to monitor for DR. OCT helps to measure retinal thickness, which is particularly valuable when there is a clinical suspicion of macular edema. The location and appearance of macular edema can be characterized with an analysis of the images. Furthermore, OCT angiography (OCT-A), which enables imaging modality for 3-dimensional visualization of retinal and optic nerve capillary network, can help to identify microaneurysms, arteriolar wall staining, retinal neovascularization, and intraretinal microvascular abnormalities. (6)
Fluorescein Angiography
Although OCT and OCT-A are increasingly used due to their non-invasive nature, the gold standard for evaluating macular ischemia and edema is fluorescein angiography. However, it is costly, time-consuming, requires venipuncture, and even poses risks of anaphylaxis and death. (6)
While these tests have proven their capability to diagnose DR accurately, they focus mainly on assessing damages that are already made to the eye.
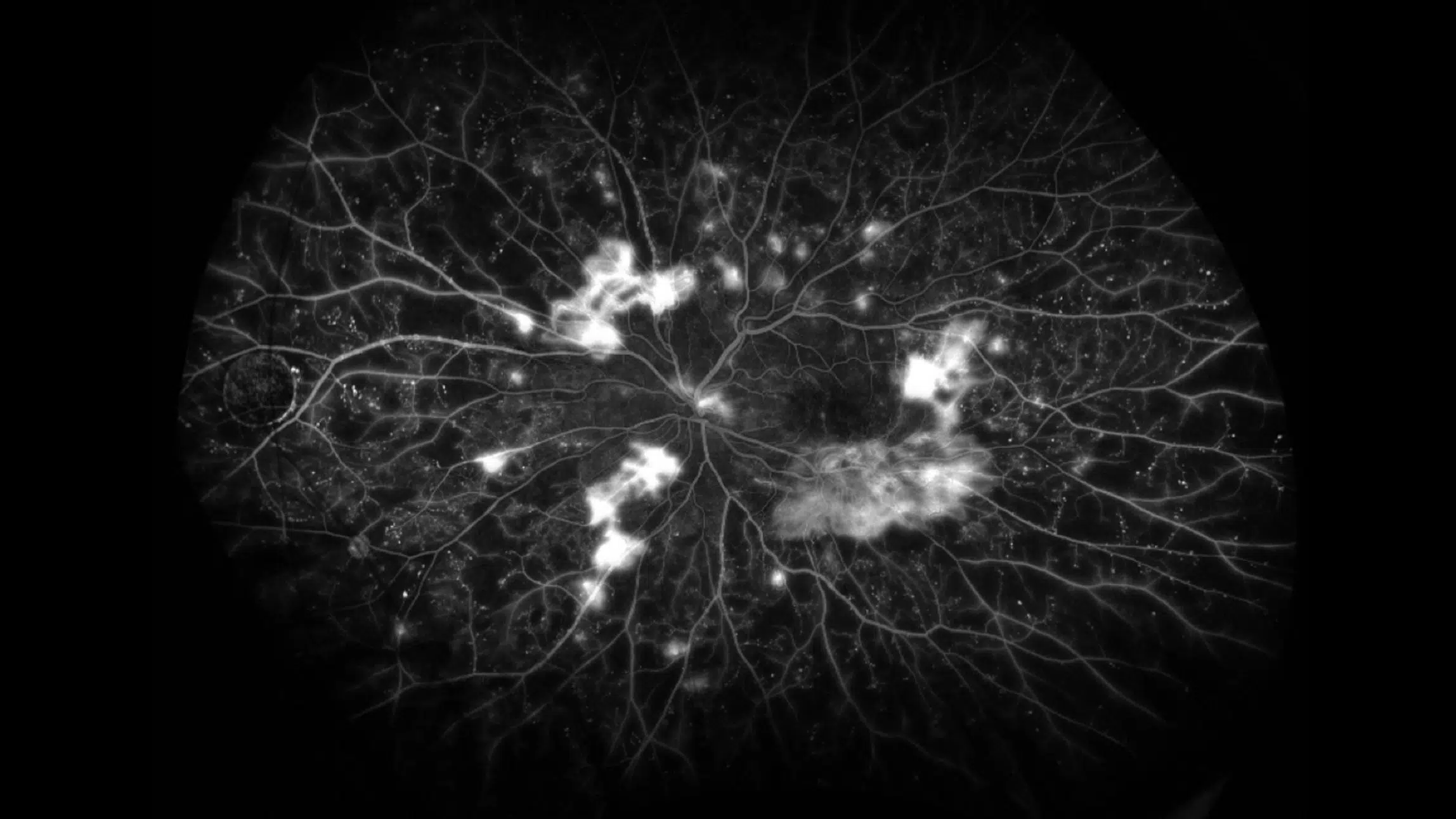
Proliferative diabetic retinopathy as seen on ultrawide-field fluorescein angiography. Source: https://collaborativeeye.com/
Ocular Oximetry
There is accumulating evidence that dysregulation of oxygen in the eye is a key indicator for loss of metabolic function and could therefore represent a crucial pathophysiological factor of DR. Thus, a major breakthrough in DR management would be the ability to measure oxygen saturation levels in order to assess metabolic changes before damages occur and help predict visual prognosis and response to treatment.
During the last years, retinal oxygen saturation has been found to be a risk factor for the development of DR. Specifically, Veibi et al studied arteriovenous oxygen saturation in young patients with Type 1 DM and found that lower levels were a risk factor for the development of NPDR. (7)
Furthermore, ocular oximetry metrics have been shown to change before measurable progression of DR can be identified. For example, oxygen saturation in larger retinal vessels can increase and the arteriovenous difference can decrease over time. This suggests that ocular oximetry is either more sensitive to these changes or that these changes precede DR progression. (8)
Thus, by using ocular oximetry to track metabolic function over time, we could significantly change the approach to preventing, screening and treating DR worldwide. New technologies such as the Zilia Ocular provide hope in this aspect as it generates new insights on the vascular health of the retina and the eye’s metabolic state. The oximetry biomarker has the potential to become an important clinical tool in DR by allowing measurement of severity of diabetic retinopathy and predicting the response to treatment.
Conclusion
The number of Americans with DR is increasing. From 2010 to 2050, this figure is expected to nearly double from 7.7 to 14.6 million. (9) DR is a treatable condition, but early intervention is key to put in place adequate treatments to prevent vision loss. New technologies give us access to unprecedented information on ocular metabolism and allow us to envision a world free from blindness caused by diabetes.
References
1. Wang W, Lo ACY. Diabetic Retinopathy: Pathophysiology and Treatments. Int J Mol Sci. 2018;19(6):1816. Published 2018 Jun 20. doi:10.3390/ijms19061816
2. Wong TY, Sabanayagam C. Strategies to Tackle the Global Burden of Diabetic Retinopathy: From Epidemiology to Artificial Intelligence. Ophthalmologica. 2020;243(1):9-20. doi:10.1159/000502387
3. Vashist P, Singh S, Gupta N, Saxena R. Role of early screening for diabetic retinopathy in patients with diabetes mellitus: an overview. Indian J Community Med. 2011;36(4):247-252. doi:10.4103/0970-0218.91324
4. Jimenez-Baez MV, Marquez-Gonzalez H, Barcenas-Contreras R, Morales Montoya C, Espinosa-Garcia LF. Early diagnosis of diabetic retinopathy in primary care. Colomb Med (Cali). 2015;46(1):14-18. Published 2015 Mar 30.
5. Murgatroyd H, Ellingford A, Cox A, et al. Effect of mydriasis and different field strategies on digital image screening of diabetic eye disease. Br J Ophthalmol. 2004;88(7):920-924. doi:10.1136/bjo.2003.026385
6. de Barros Garcia JMB, Isaac DLC, Avila M. Diabetic retinopathy and OCT angiography: clinical findings and future perspectives. Int J Retina Vitreous. 2017;3:14. Published 2017 Mar 13. doi:10.1186/s40942-017-0062-2
7. Veiby NCBB, Simeunovic A, Heier M, et al. Retinal venular oxygen saturation is associated with non-proliferative diabetic retinopathy in young patients with type 1 diabetes [published online ahead of print, 2021 Oct 20]. Acta Ophthalmol. 2021;10.1111/aos.15018. doi:10.1111/aos.15018
8. Hardarson SH, Stefánsson E, Bek T. Retinal oxygen saturation changes progressively over time in diabetic retinopathy. PLoS One. 2021;16(5):e0251607. Published 2021 May 12. doi:10.1371/journal.pone.0251607
9. Nei.nih.gov. n.d. Diabetic Retinopathy Data and Statistics | National Eye Institute. [online] Available at: <https://www.nei.nih.gov/learn-about-eye-health/outreach-campaigns-and-resources/eye-health-data-and-statistics/diabetic-retinopathy-data-and-statistics>
Written by the Zilia Team on November 26, 2021
More on our Blog
Zilia Partners with Kagawa University for Groundbreaking Retinal Oxygenation Study in Japan
Quebec City, Apr. 30, 2024 - Zilia, a pioneer in non-invasive ocular biomarker technologies, announces a...
Oxygen’s Complex Role in Retinopathy of Prematurity
Premature birth is a remarkable feat of medicine. However, this early entrance into the world can sometimes...
Oxidative Stress and Eye Health
Oxygen plays an important role in our universe, being the third most abundant element and the second most...
Solutions